Tag Archives: health
Link
/* Style Definitions */
table.MsoNormalTable
{mso-style-name:”Table Normal”;
mso-tstyle-rowband-size:0;
mso-tstyle-colband-size:0;
mso-style-noshow:yes;
mso-style-priority:99;
mso-style-qformat:yes;
mso-style-parent:””;
mso-padding-alt:0cm 5.4pt 0cm 5.4pt;
mso-para-margin-top:0cm;
mso-para-margin-right:0cm;
mso-para-margin-bottom:10.0pt;
mso-para-margin-left:0cm;
line-height:115%;
mso-pagination:widow-orphan;
font-size:11.0pt;
font-family:”Calibri”,”sans-serif”;
mso-ascii-font-family:Calibri;
mso-ascii-theme-font:minor-latin;
mso-fareast-font-family:”Times New Roman”;
mso-fareast-theme-font:minor-fareast;
mso-hansi-font-family:Calibri;
mso-hansi-theme-font:minor-latin;}
Thank you Dr Verner Wheelock for the extensive critique of the reports . The Cochrane reports analysis was heroic and well structured. We had a huge debate about them at the time on THINCS (www.thincs.org).
For my part I shy away from statistical analysis which doesn’t include ‘All Cause Mortality’ figures. The reason being that failure to look at all the non-cardio deaths and drop-outs from trials cleans and amplifies the apparent benefits of Statins. This means we can never know the Numbers Needed to Harm NNH side of the medication.
My first ever review paper (G Wainwright et al., 2009) looking at the clinical impact of cholesterol lowering in all non-cardiovascular organs, was seminal in that it pointed up a fundamental flaw in the whole statin concept i.e. Cholesterol is vital and inhibiting its production is destined to create a wide and varied set of Adverse Events in statin users in the longer term. That is why ‘all cause mortality’ data is not made available (caveat emptor).
In our second review paper(Seneff et al., 2011) we became aware of the fact that LDL/HDL ratios were associated with LDL consumption by organs and not production by the liver. The whole LDL argument had been inverted. If LDL is damaged by glycation, LDL goes up and HDL falls. The liver’s glycated-LDL is unused and the corresponding HDL return to the liver does not happen.
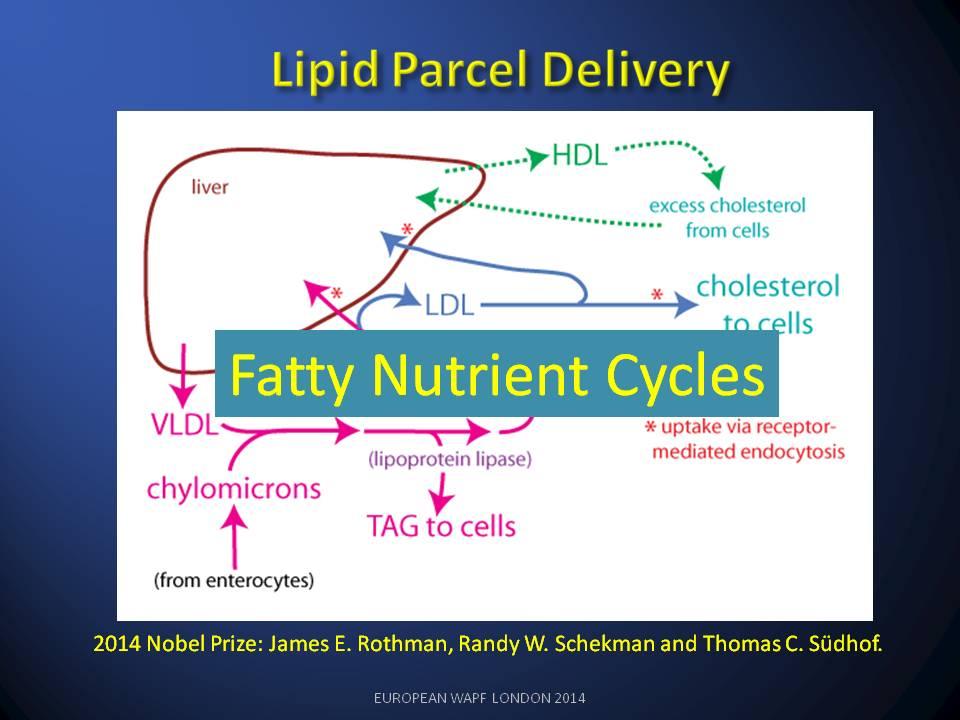
How such a fundamental part of the lipid nutrition cycle could be missed is hard to understand. Obsession with statins and statin finance has done immense harm to cardio-medicine and I believe we are seeing the start of a major NICE scandal as the BMA object to the guidance.
Link
The treatment and placebo groups’ mortality lines should be independent: a trend in one should have no consequential influence on the other. However:
- All 4 lines are essentially identical for 1.6 years.
- Then there is a departure — by both lines at the same time.
The fact that both lines — treatment and placebo — depart at the same time is important. Why should the treatment suddenly become beneficial at exactly the same time as non-treatment becomes detrimental?
The average line of both treatment and non-treatment groups follows a ‘natural’ mortality curve; any natural survival curve would have its slope increasing downward. (i.e. becoming more negative.)
Both treatment and placebo lines follow this natural curve for 1.6 years. Then both diverge. The placebo group shows this slope change increasing (negative) at a faster rate than all other lines. But, surely, it should follow the natural mortality curve. Why doesn’t it?
The slope of the treatment group is nearly constant from 1.8 years onward. It’s not a curve at all, but an almost straight line — and it shouldn’t be. What it says is that old people die at the same rate as younger ones. And life isn’t like that.
Is this evidence that the data of the 4S trial were not handled in an honest manner? Were deaths occurring in the treatment group assigned to the placebo group? Is this why the two curves, which should be independent, are apparently related? Or is there a mistake somewhere? Is there an error in logic?
Sugar-Damage in the Lipid Nutrition Cycle
Normal
0
false
false
false
false
EN-GB
X-NONE
X-NONE
/* Style Definitions */
table.MsoNormalTable
{mso-style-name:”Table Normal”;
mso-tstyle-rowband-size:0;
mso-tstyle-colband-size:0;
mso-style-noshow:yes;
mso-style-priority:99;
mso-style-qformat:yes;
mso-style-parent:””;
mso-padding-alt:0cm 5.4pt 0cm 5.4pt;
mso-para-margin-top:0cm;
mso-para-margin-right:0cm;
mso-para-margin-bottom:10.0pt;
mso-para-margin-left:0cm;
line-height:115%;
mso-pagination:widow-orphan;
font-size:11.0pt;
font-family:”Calibri”,”sans-serif”;
mso-ascii-font-family:Calibri;
mso-ascii-theme-font:minor-latin;
mso-fareast-font-family:”Times New Roman”;
mso-fareast-theme-font:minor-fareast;
mso-hansi-font-family:Calibri;
mso-hansi-theme-font:minor-latin;}
Maybe raised total blood serum cholesterol (TBSC) was trying to tell us something about health, but it was not the message we have been fed for the last 60 years.
Cholesterol has been misrepresented since the 1950s as a cause of heart disease. In reality an excess of dietary sugar that created an unhealthy lipid profiles in our blood stream. Attempts to fix the problem by a drug called a statin added to our health woes because it targets the wrong issue.
When LDL nutrition is sugar-damaged (Glycated LDL) is raised in the blood. Unrecognised by our fat starved organs it is eventually scavenged by less discriminating visceral fat stores. There is less HDL (erroneously called ‘good’ cholesterol) being returned by the organs.
High Cholesterol (high levels of total blood serum cholesterol TBSC) when caused by damage to the LDL lipid parcels is a sign that lipid circulation is broken. These fats (LDL) will be scavenged to become visceral fats, deposited around the abdomen. This type of damage is associated with poor health.

Preventing the liver from producing new undamaged LDL by using a statin fails to address the problem of getting fatty nutrients to fat starved organs. The action of statins adds to the patients musculo-skeletal and neurological woes by depleting vital supplies of CoQ10 and dolichol.
The problem is fixed by reducing sugar-damage – as measured by an HbA1c test on sugar damage to a blood protein called haemoglobin. Several diabetes clinicians have observed this key connection between sugar damage and poor lipid profiles.
A Healthy Lipid Nutrition Cycle

If the total blood serum cholesterol (TBSC) is high and the organs are getting enough lipids, the blood lipid circulation is healthy. The large parcels of fatty nutrients (LDL lipids) sent by the liver are consumed by our organs (receptor-mediated endocytosis) and the smaller fatty wrappers and left-over lipids (HDL Lipids) return to the liver. The Fatty Nutrients (LDL) and the recycled lipids (HDL) are in balance. Such a healthy-lipid ‘High-Cholesterol’ person is well nourished and likely to have a long and healthy life.
Sugar-Damage in a Broken Lipid Cycle

If the total blood serum cholesterol is high but the fatty nutrient droplets (LDLs) have sugar-damaged labels, the organs are unable to recognise and feed on them. The supply of fatty nutrients to organs is broken.
The liver continues to supply fatty nutrients (albeit with damaged LDL labels), but the organs’ receptors are unable to recognise them. The organs thus become starved of their fatty nutrients. Like badly labelled parcels in a postal service, the sugar-damaged lipids build up in the blood (raised LDL) and fewer empty wrappers are returned to the liver (low HDL).
So it really doesn’t matter how high your total blood serum cholesterol (TBSC) is. What really counts is the damaged condition of the blood’s fatty nutrient parcels (LDL lipids). In our research review of metabolic syndromes4 (e.g. diabetes, heart disease, obesity, arthritis and dementia) we explained that the major cause of lipid damage was sugar-related.
Sugar Damage (AGEs)
The abbreviation AGE (Advanced Glycation End-product) is used to describe any sugar-damaged protein. As we age, excessive amounts of free sugars in the blood5 may eventually cause damage quicker than the body can repair it. The sugars attach by a chemical reaction and the sugar called fructose is known to be 10 times more reactive, and therefore more dangerous than our normal blood sugar (glucose). Since the 1970s we have been using increasing quantities of refined fructose (from high-fructose corn syrup). Its appealing sweetness, and ability to suppress the ‘no longer hungry’ receptor6 (ghrelin receptor) is driving excessive food intake. Its ability to damage our fatty nutrients and lipid circulation is also driving waist-line obesity and its associated health problems4,7.
Checking for Damage in our Lipids
There is a ‘simple to administer’ commonly available blood test used to check for sugar-damage. It is used to check the proteins in the blood of people who are diabetic or at risk of becoming diabetic. It tests for Glycated Haemoglobin (HbA1c) by counting the proportion of damaged molecules (per 1000) of Haemoglobin protein in the blood (mmol/mol). Researchers looking at ways of testing for damage to lipids, have found that sugar-damaged blood protein test (HbA1c), presents a very reasonable approximation of the state of sugar-damage in the blood lipids. Until there is a good general test for sugar-damage in blood lipids, this test (HbA1c) could be a sensible surrogate. This is a better way of assessing health than a simple cholesterol test (TBSC).
Improved sugar-damaged blood protein (HbA1c) scores in diabetic patients is accompanied by improvements in their lipid profiles. This could be very useful to anyone wanting to improve health outcomes by managing lifestyle and nutrition.
For the full essay with references read follow this ‘bitly link’: http://bit.ly/1fkGYgb
Link
The Paradox
For over 50 years this has been a paradox, the ‘High-Cholesterol Paradox’. What is really going on?

Hypothesis becomes Dogma

Let us explore some more big anomalies in the last 40 years of dietary health guidance.
Good Cholesterol? Bad Cholesterol? Spot the Difference?

Healthy Lipids

Damaged Lipids

Sugar Damage (AGEs)
Checking for Damage in our Lipids
Clinical Consequences of Lowering Cholesterol
Memories are made of this – Cholesterol
Consequences of Lowering Cholesterol
Our review12 found that cholesterol lowering therapies were implicated in:
· Damage to muscles (including the heart) and exercise intolerance13
· Increased risk of Dementias (Impaired Synaptogenesis and Neuro-transmission)14
· Failure of Myelin Maintenance (Multiple Sclerosis Risks)15
· Neuro-muscular problems, aches and pains (Amyotrophic Lateral Sclerosis)16
· Diabetes (Insulin release inhibited)8
· Poor Maintenance of Bones and Joints
· Suppression of protective skin secretions (Apo-B) and increased MRSA infection17
Why would anyone want to lower cholesterol?
What is needed is a lowering of damage to lipids – caused by sugar.
3. Yudkin, J. Pure, white and deadly: how sugar is killing us and what we can do to stop it. (2012).
The ‘High Cholesterol’ Paradox
Link
Sweden has become the first Western nation to develop national dietary guidelines that reject the popular low-fat diet dogma in favor of low-carb high-fat nutrition advice.
Some quotes from Prof. Nyström translated into English from Dr. Eenfeldt:
Butter, olive oil, heavy cream, and bacon are not harmful foods. Quite the opposite. Fat is the best thing for those who want to lose weight. And there are no connections between a high fat intake and cardiovascular disease.
On Monday, SBU, the Swedish Council on Health Technology Assessment, dropped a bombshell. After a two-year long inquiry, reviewing 16,000 studies, the report “Dietary Treatment for Obesity” upends the conventional dietary guidelines for obese or diabetic people.
For a long time, the health care system has given the public advice to avoid fat, saturated fat in particular, and calories. A low-carb diet (LCHF – Low Carb High Fat, is actually a Swedish “invention”) has been dismissed as harmful, a humbug and as being a fad diet lacking any scientific basis.
Instead, the health care system has urged diabetics to eat a lot of fruit (=sugar) and low-fat products with considerable amounts of sugar or artificial sweeteners, the latter a dangerous trigger for the sugar-addicted person.
This report turns the current concepts upside down and advocates a low-carbohydrate, high-fat diet, as the most effective weapon against obesity.
The expert committee consisted of ten physicians, and several of them were skeptics to low-carbohydrate diets at the beginning of the investigation.
Link
More debunking of alarmist medical research from Zoe.
Link
Link to petition and it seems Fructose is the bad guy
Law enforcement for a health warning for dietary sugar – a petition
Link
Earlier this year I attended a the London WAPF conference in support of Dr Stephanie Seneff and we were fortunate enough to meet Dr Natasha Campbell-McBride. Once Dr Natasha C-M explains what happens to the food you eat and how it affects your health you are empowered to improve your health. She asks you to consider the community that lives within us digesting our food and protecting us from infection and harm. Once you understand your symbiotic relationship with this microbial community you will respect it, nurture it and take much greater care of what you put in your mouth.
e.g. If food manufacturers treat food to extend its shelf-life (the spoilage bugs can’t survive on it) you have to consider what that does to your internal community of microbial friends when you eat it!




