
Forty years ago Henry Gadsden, chief executive of the drug company Merck, expressed his frustration that the potential market for his company’s products should be limited to those with treatable…
Ever since I read Medical Myths by Joel Kauffman, I have had trouble believing that treating Blood Pressure with one of 5 different chemicals did anything to address the cause of raised blood pressure. Blood pressure is raised by glycation of arterial proteins (Sugar-Damage) how does a pill other than maybe metformin address that? Lo-Carb Hi-Fat LCHF will address that issue eventually but best not get glycated to start with!
The Independent.ie said today:-
And the source of this story is here
“Even if only 10 per cent of doctors followed the guidelines, and that is a conservative estimate, 100 million patients would have been given beta blockers during surgery in the past decade. On the basis of our findings, that means 800,000 would have died prematurely and 500,000 would have suffered a stroke. If our findings are true, that is death on the scale of a world war.” Devereaux P J Associate Professor, Department of Clinical Epidemiology and Biostatistics Mc Master University


As experts clash over proposals that millions more of us take statins to prevent heart disease and stroke, a vascular surgeon explains why he feels better without them
You can also read my related essay on this link http://bit.ly/1fkGYgb
http://www.theguardian.com/commentisfree/2014/mar/23/statins-not-wonder-drug-major-diseases
For over 50 years this has been a paradox, the ‘High-Cholesterol Paradox’. What is really going on?


Let us explore some more big anomalies in the last 40 years of dietary health guidance.



Our review12 found that cholesterol lowering therapies were implicated in:
· Damage to muscles (including the heart) and exercise intolerance13
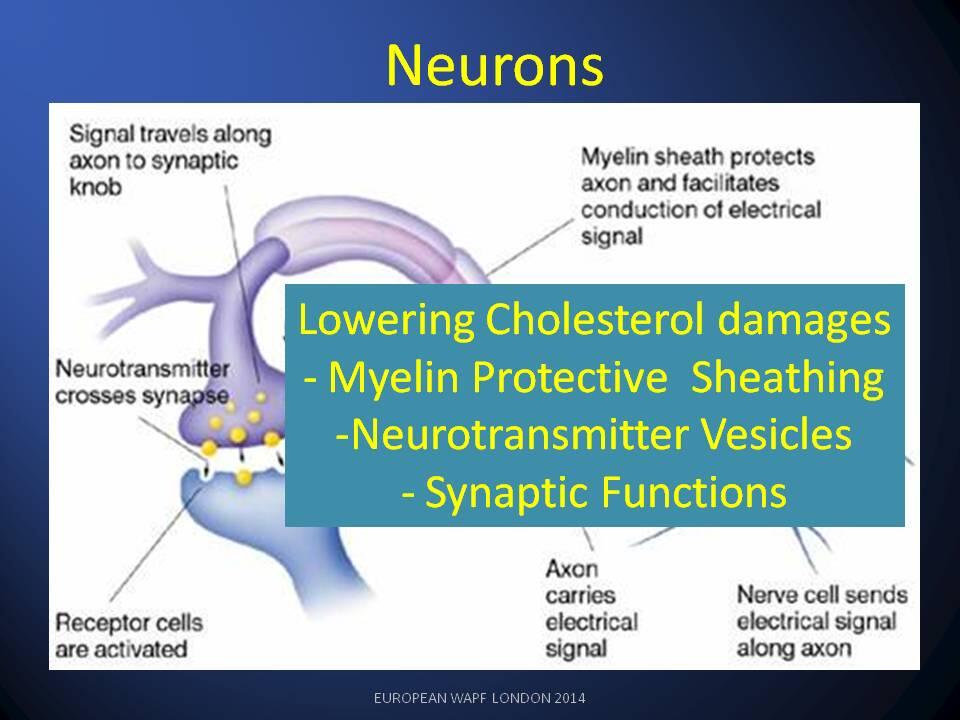
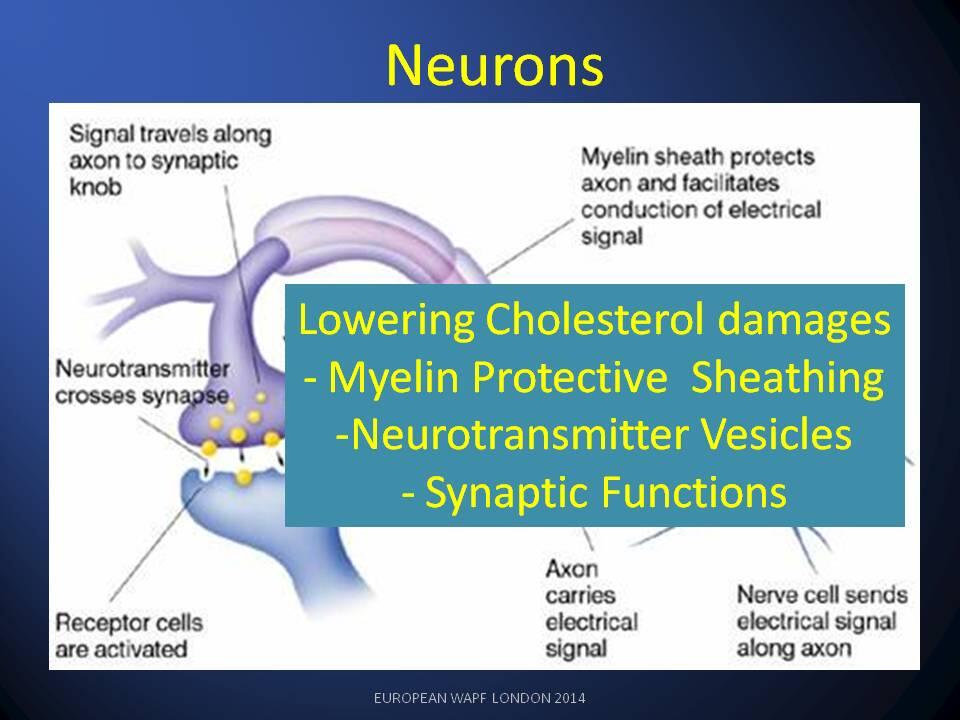
· Increased risk of Dementias (Impaired Synaptogenesis and Neuro-transmission)14
· Failure of Myelin Maintenance (Multiple Sclerosis Risks)15
· Neuro-muscular problems, aches and pains (Amyotrophic Lateral Sclerosis)16
· Diabetes (Insulin release inhibited)8
· Poor Maintenance of Bones and Joints
· Suppression of protective skin secretions (Apo-B) and increased MRSA infection17
Why would anyone want to lower cholesterol?
What is needed is a lowering of damage to lipids – caused by sugar.
3. Yudkin, J. Pure, white and deadly: how sugar is killing us and what we can do to stop it. (2012).
A sample preview of slides for my presentation is linked here.
Publications on which the talk is based are free to download here.

The Bio-chemical Science pages of Glyn Wainwright, Publisher, Independent Reader of Research and Honorary Recording Engineer for Leeds Symphony Orchestra<
Anecdote: A diabetic clinician told me she had noticed that when patients had good control of their hba1c (an indicator of sugar-damage in blood ) their ‘cholesterol’ score also improved.
Every molecule of cholesterol in the body is known to be identical to every other.
The Good/Bad labeling of cholesterol is extremely unscientific and unhelpful, and that is a matter of scientific fact.
How were intelligent, well educated, medical professionals persuaded to popularise this ‘Good ‘ cholesterol versus ’Bad’ cholesterol idea?
The unscientific phrase ‘Bad Cholesterol’ is a misleading description of damage to the ’lipid transport system ‘, whose basic function was described by the Nobel Prize winners James E. Rothman, Randy W. Schekman and Thomas C. Südhof. (Awarded “for their discoveries of machinery regulating vesicle traffic, a major transport system in our cells”.
The lipid transport system is used by the body to deliver essential supplies of fat, cholesterol, and other fat-soluble nutrients.
The lipid transport system is able to repair and recycle, but can be progressively overwhelmed by the damage accumulated over several decades.
This damage to the lipid system is caused by oxidation and glycation: the result of excessive consumption of refined sugars (in particular High Fructose syrups).
It is not ‘bad cholesterol’ but sugar-damage to the proteins that make the lipids available to the organs of our body.
Unconsumed ‘damaged’ ldl in the blood is an indicator of trouble because the organs are being starved of vital fats cholesterol and fat-soluble nutrients.
‘Bad Medicine’ prevents the liver and all other organs from making essential cholesterol indirectly stop the supply of lipids to the blood.
Cholesterol lowering medications have a variety of very broad variety of adverse-effects, all attributable to organs being starved of fat, cholesterol and fat-soluble nutrients.
The ‘bad medicine’s do not tackle the cause of damage to the ldl – lipids supply.
The primary cause of this ldl damage is the oxidation and glycation of the ldl’s components.
The main dietary and lifestyle causes of ldl damage are over-consumption of refined sugars and inactivity.
The reactive sugars like fructose, found in manufactured corn syrups are particularly troublesome, because they directly attach to ldl-protein mechanisms causing a mal-function which starves the organs.
Important protective and anti-oxidant functions rely on Cholesterol and CoQ10 – both of which are reduced anti-cholesterol medications.
The unscientific use of the incorrect description ‘Bad Cholesterol’ has held back medicine for over 40 years and it is time to look at the evidence in more detail:-